Early Assessment and Early Intervention are required
Ovarian cancers are most often diagnosed when they are already advanced and difficult to treat.
In 2021, there were an estimated 238,484 women living with ovarian cancer in the United States.
According to the National Cancer Institute over 50% of all women diagnosed with ovarian cancer die of this disease within 5 years. These are tragic statistics.
Approximately 1.1 percent of women will be diagnosed with ovarian cancer at some point during their lifetime, based on 2018–2021 data, excluding 2020 due to COVID.
Symptoms of ovarian cancer can be hard to identify as they are vague and often resemble other common conditions. Pap smears are not diagnostic and routine pelvic exams do not typically detect ovarian cancer at early stages.
But new study* shows promising signs ovarian cancer can be detected in its early stages. The study targeted women with four specific symptoms – bloating, abdominal pain, needing to pee frequently, and feeling full quickly – and put them on a fast track to see a specialist.
As a result, even the most aggressive forms of ovarian cancer could be detected in their early stages.

Frequently primary care providers will not take crucial step to RULE OUT ovarian cancer and often assume the woman is having only digestive, genito-urinary or menstrual symptoms. It is crucial to look for ovarian cancer even when symptoms are mild and appear similar to common conditions. After all, ovarian cancer is life threatening, hard to treat in advanced stages and takes the lives of many women.
So, what did the study find? And what could it mean for detecting – and treating – ovarian cancer more quickly?

Why is ovarian cancer hard to detect early?
Current gynecology guidelines state that women get tested for ovarian cancer only if they have symptoms for more than one month. But many of the symptoms of ovarian cancer such as tiredness, constipation and changes in menstruation – are vague and overlap with other common illnesses. Women must be taken seriously as reliable reporters of significant changes in their bodies and clinicians should not diminish their reporting. Rather than take a wait and see approach, a proactive, initiation of a diagnostic process should ensue without delay.
If diagnosed at Stage 1 and confined to the primary site with no spread, the five-year survival rate is 92%. This makes early detection critical.
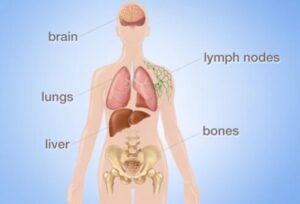
Survival rates are linked to the stage at diagnosis. Most women are diagnosed at Stage 3 or 4 with metastatic advanced disease. If the cancer has spread to nearby lymph nodes, the survival rate is reduced to 72%. If the cancer has already metastasized and spread to distant sites at the time of diagnosis, the rate is only 31%.
Monitoring four key symptoms
Between June 2015 and July 2022, the researchers recruited 2,596 women aged between 16 and 90 from 24 hospitals across the UK.
They were asked to monitor for these four symptoms:
- persistent abdominal distension (women often refer to this as bloating)
- feeling full shortly after starting to eat and/or loss of appetite
- pelvic or abdominal pain (which can feel like indigestion)
- needing to urinate urgently or more often.
Women who reported at least one of four symptoms persistently or frequently were put on a “fast track pathway”. That means they were immediately referred to and seen by a gynecologist within two weeks.
A cancer antigen 125 (CA125) blood test was performed. (Positive in some but not all ovarian cancers). And the patient also received a transvaginal pelvic ultrasound to visualize the ovaries and the pelvis.
Findings
Some 12% of women on the fast-track pathway were diagnosed with some kind of ovarian cancer.
A total of 6.8% of fast-tracked patients were diagnosed with high-grade serous ovarian cancer. It is the most aggressive form of cancer and responsible for 90% of ovarian cancer deaths.
Out of those women with the most aggressive form, one in four were diagnosed when the cancer was still in its early stages. That is important because it allowed treatment of the most lethal cancer before it had spread significantly through the body.
There were some promising signs in treating those with this aggressive form. The majority (95%) had surgery, and three quarters (77%) had chemotherapy. Complete cytoreduction – meaning all the cancer appears to have been removed – was achieved in six women out of ten (61%).
Because women may receive a thorough gynecologic exam only once every 1-2 years, this contributes to late diagnosis. Furthermore, it is often the primary care provider who first hears complaints of fatigue, bloating, urinary frequency, dull abdominal pain, changes in bowel function, pain with intercourse. It is the primary care provider who should take action and order a CA125 and a pelvic ultrasound.

What does this mean for detection?
The study’s findings suggest this method of early testing and referral for the symptoms leads to earlier detection of ovarian cancer
This study points to the importance of public awareness and primary care provider awareness about symptoms and timely assessment.
Clinicians should be able to recognize all the ways ovarian cancer can present, including vague symptoms like general fatigue.
Empowering women to recognize a set of four symptoms can help trigger testing, detection and treatment of ovarian cancer earlier. Women can also ASK FOR serum testing and pelvic ultrasound and a thorough and thoughtful gynecologic workup.
Many women as well as many primary care providers remain unaware of early signs and symptoms of ovarian cancer. This study shows recognizing and reporting symptoms early and taking action to measure serum CA-125 and perform a pelvic ultrasound may help early detection and treatment and improve survival rates.
The OutSmart Cancer® System promotes regular screenings, early assessment and early intervention, empowering both patients and their primary care and specialty care providers to engage in a pro-health model. With ovarian cancer, this saves lives.
Selected References
*Kwong FLA, et al. Int J Gynecol Cancer 2024;0:1–7. doi:10.1136/ijgc-2024-005371 Symptom-triggered testing detects early stage and low volume resectable advanced stage ovarian cancer
Ovarian Cancer: The Recognition and Initial Management of Ovarian Cancer. Cardiff (UK): National Collaborating Centre for Cancer (UK); 2011 Apr. PMID: 22479719.
Brain KE, Smits S, Simon AE, Forbes LJ, Roberts C, Robbé IJ, Steward J, White C, Neal RD, Hanson J; ICBP Module 2 Working Group. Ovarian cancer symptom awareness and anticipated delayed presentation in a population sample. BMC Cancer. 2014 Mar 10;14:171. doi: 10.1186/1471-2407-14-171. PMID: 24612526; PMCID: PMC3975332.
Bloomfield HE, Olson A, Greer N, Cantor A, MacDonald R, Rutks I, Wilt TJ. Screening pelvic examinations in asymptomatic, average-risk adult women: an evidence report for a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2014 Jul 1;161(1):46-53. doi: 10.7326/M13-2881. PMID: 24979449.